ARTICLE SUMMARY: Hydrocodone is a prescription painkiller prescribed for moderate pain. However, it can also be addictive, causing long term changes in brain function.
TABLE OF CONTENTS
- Long-Term Definition
- Body Effects
- Statistics and Over-Prescription
- Signs of a Problem
- No Stigma
- Next Steps
Long term Definition
The medical definition for “long-term” prescription can vary. Some experts consider anything more than one month to be “long-term” use. Other markers may be 3-6 months, but usually never more than that. In medical studies, an episode of long-term use is defined as at least 3 prescriptions issued within a 90-day period from the date of an initial prescription. Episodes of long-term use typically end when there is a gap of 6 months or more without a prescription.
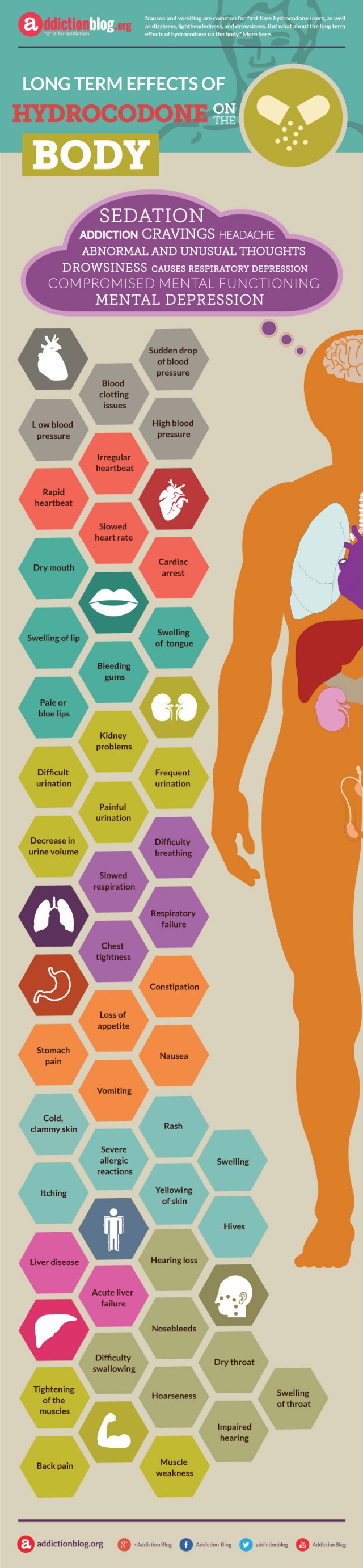
Body Effects
Primary effects of hydrocodone on the brain
- pain relief
- drowsiness
- respiratory depression
- sedation
Secondary effects of hydrocodone on the brain
- compulsion
- compromised mental functioning
- cravings
- headache
- mental depression
Cardiovascular system effects
- blood clotting issues
- high blood pressure
- low blood pressure
- sudden drop of blood pressure
Heart effects
- cardiac arrest
- irregular heartbeat
- rapid heartbeat
- slowed heart rate
Mouth effects
- bleeding gums
- dry mouth
- pale or blue lips
- swelling of tongue
- swelling of lip
Kidney effects
- decrease in urine volume
- difficult urination
- frequent urination
- kidney problems
- painful urination
Effects on the Lungs
- chest tightness
- difficulty breathing
- respiratory failure
- slowed respiration
Digestion
- constipation
- loss of appetite
- nausea
- stomach pain
- vomiting
Skin Effects
- cold, clammy skin
- hives
- itching
- rash
- severe allergic reactions
- swelling
- yellowing of skin
Liver Effects
- acute liver failure
- liver disease
Damage to the Ear, Nose and Throat
- difficulty swallowing
- dry throat
- hearing loss
- hoarseness
- impaired hearing
- nosebleeds
- swelling of throat
Muscles
- back pain
- muscle weakness
- tightening of the muscles
Statistics and Over-Prescription
If you’re worried about using hydrocodone and its effects, you are not alone! The 2016 National Survey of Drug Use and Health (NDSUH) found that hydrocodone is one of the most popular prescriptions medications in the U.S. The 2016 NSDUH findings estimate that:
- 54.8 million people used a medicine containing hydrocodone in the last year.
- 6.9 million people reported misuse of hydrocodone in the last year.
In fact, this 2014 study published in the American Journal of Epidemiology reported that hydrocodone was reponsible for an increasing number of overdose deaths in the U.S. Further, this IMS Health, National Prescription Audit (NPATM) presentation shows how hydrocodone is over-prescribed. In fact, providers wrote nearly a quarter of a billion painkiller prescriptions in 2013, enough for every American adult to have their own bottle of pills.
Addiction to hydrocodone can happen quickly or can develop slowly, over time. Who’s at risk of a hydrocodone problem?
- People taking high doses.
- People who use it to get high.
- People who doctor shop for more prescriptions.
- People with a medical history of addiction.


In 2014, nearly two million Americans either abused or were dependent on prescription pain relievers like hydrocodone.
Signs of a Problem
While many people start taking hydrocodone as prescribed, around one in ten people who use this powerful painkiller end addicted to it. Drug dependence makes it even more difficult to quit hydrocodone on your own. So, if you find yourself with a hydrocodone problem, what do you do?
First, you can admit you have a problem. The main signs of a hydrocodone problem are:
- Increased tolerance.
- Needing hydrocodone to feel normal.
- Using hydrocodone despite negative effects on health, home, or work.
- Using hydrocodone to get high.
- Quitting, but having difficulty staying quit.
You can find a list of full signs and symptoms of hydrocodone addiction via this Addiction Blog article.
Then, you start looking for help. You can speak with your prescribing doctor for an initial drug addiction assessment. These drug problem screening tools from the U.S. Department of Health and Human Services are a good place to start.
No Stigma
Anyone who takes prescription opioids can become addicted to them. So, if you are experiencing problems with hydrocodone…there is nothing to be ashamed of. In fact, this 2009 study published in the medical journal, Drug and Alcohol Dependency reported that, “as many as one in four patients receiving long-term opioid therapy in a primary care setting struggles with opioid addiction.“
But once you’re addicted, it can be hard to stop. The brain goes through changes and it continues to seek hydrocodone to regulate its functions and behaviors. If you find yourself in this circle and want to quit, you may need medical help. Hydrocodone addiction is a medical condition. You’ll need a diagnosis before experts know what treatments may be appropriate
What Next?
If you want to get off hydrocodone for good, you have a few options.
1. Seek an addiction diagnosis. You can find help with your prescribing physician, a psychiatrist, an addiction specialist (MD), a licensed clinical psychologist, a licensed clinical social worker, or in an addiction treatment center.
2. Go through hydrocodone detox. If you have become physically dependent on hydrocodone, you’ll need to slowly wean yourself off the pain medication. There are specific tapering guidelines that you can follow during this process. Generally, dose reduction happens over the course of a few weeks with stabilization periods of a few days before you step-down doses.
3. Learn how to cope without hydrocodone. Physical dependence is one thing. Psychological dependence is another. Once you get hydrocodone out of your system, you’ll need to learn without it. Often, this involves behavioral changes in how you deal with stress, anxiety, and/or anger. Life training skills through psychotherapy help. So does exploring past issues related to trauma or emotional problems.
KNOW THIS: You are not alone!
If you’re noticing body changes related to your hydrocodone…get help now. You don’t need to suffer in silence. And, you don’t need to deal with the problem alone.








Related Posts